NAFLD to MAFLD
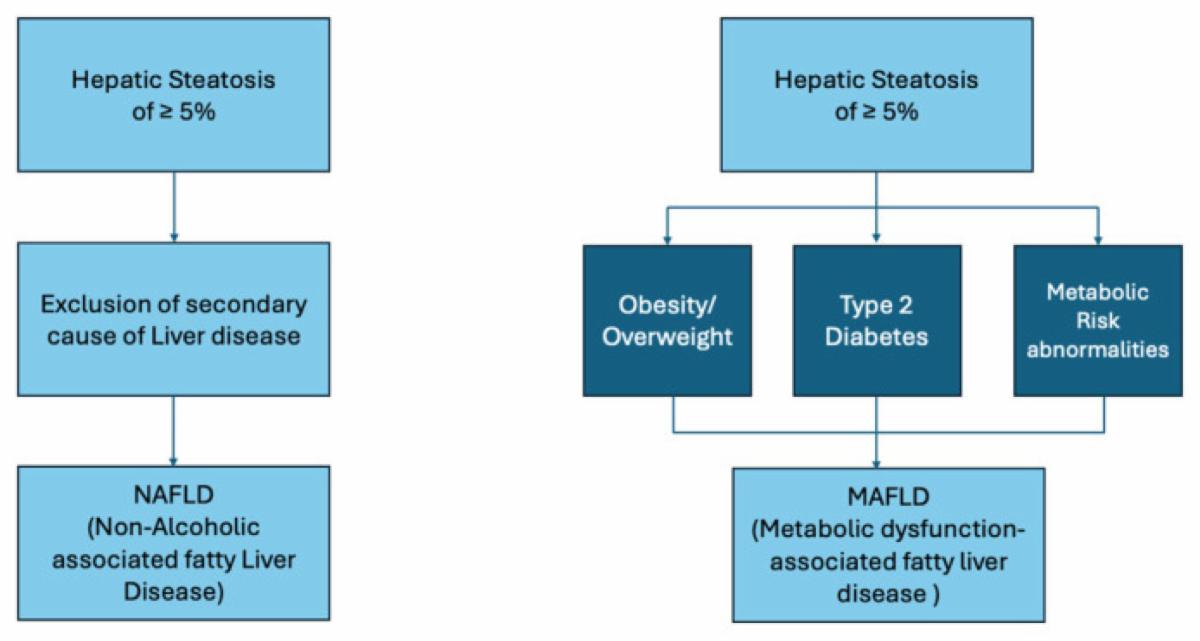
Non-alcoholic fatty liver disease (NAFLD) is defined as a chronic liver disease characterized by excessive fat accumulation in the liver without another obvious cause (no excessive alcohol consumption, hepatotoxic
medications, toxins, viral infections, genetic hepatic diseases), therefore it is an exclusion diagnosis. The term NAFLD literally refers to non-alcohol related hepatopathy and does not adequately correlate with metabolic dysfunction and related cardiovascular risks. Therefore, researchers and scientific societies have moved towards changing the terminology. The novel nomenclature for a metabolic-associated fatty liver disease (MAFLD) has been proposed in 2020 by a group of experts to overcome the issues related to the old terminology. The diagnosis of MAFLD is based on the presence of hepatic steatosis and at least one between these three conditions: type 2 diabetes mellitus (T2DM), obesity or metabolic dysregulation (Boccatonda et al., 2023).
Metabolic dysfunction-associated fatty liver disease (MAFLD) is a growing global health concern which is driven by the increasing prevalence of diabetes and obesity. MAFLD is characterized by excessive fat accumulation in the liver, which encompasses a range of conditions, from simple hepatic steatosis to more severe forms. This condition is associated with various complications, including chronic kidney disease (CKD), Cardiovascular Disease (CVD), liver cirrhosis, and even malignancy. Recent research has highlighted a potential connection between gut dysbiosis and MAFLD, particularly in relation to CKD. This has underscored the significance of the gut-liver-kidney axis in understanding MAFLD's pathogenesis. Inflammation triggered by MAFLD increases the risk of CVD through multiple mechanisms linked to metabolic dysfunction. These mechanisms include heightened oxidative stress, systemic and hepatic insulin resistance, low-grade inflammation, and endothelial dysfunction. Hepatic steatosis and metabolic dysfunction are major diagnostic criteria for MAFLD, often coexisting with other liver ailments.
Metabolic risk abnormalities
- Waist circumference of >102/88 cm in Caucasian men and women
and >90/80 cm in Asian men and women. - Blood pressure of 130/85 mmHg or treatment for hypertension
- Plasma triglycerides of 1.7 mmol/L or specific drug treatment.
- Plasma high-density lipoprotein <1.0 mmol/L for men and <1.3
mmol/L for women or specific treatment. - Conditions for prediabetes: fasting plasma glucose 5.6–6.9 mmol/L,
2-h post-load glucose levels 7.8–11.0 mmol/L, or HbA1c 5.7%–6.4%. - Homeostasis model assessment of insulin resistance score >2.5. 7
|
|
|